Blue Cross Blue Shield of North Dakota (BCBSND) continues to utilize Change Healthcare’s InterQual® criteria sets. BCBSND has received updated criteria (2023 Release Criteria) and will start using version 2023 criteria for dates of service November 1, 2023, and later.
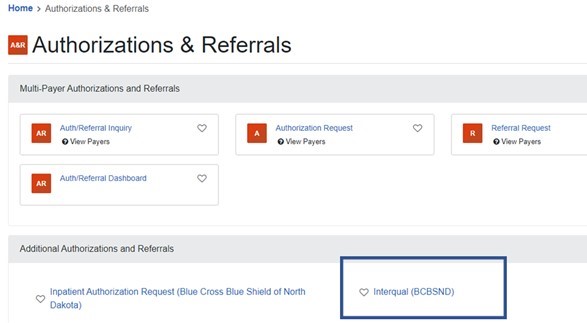
InterQual® criteria sets are via the InterQual® (BCBSND) link on the Availity Essentials portal under the Authorizations & Referrals section.
- August 17, 2023
- Education
2023 InterQual Criteria Implementation-Updated
InterQual® exceptions can be made to reflect organizational needs such as legislative or geographic differences. BCBSND does identify the below organizational exceptions for primary reviewers. These exceptions will be reviewed annually with InterQual® version updates.
Episode Day Inpatient Criteria – The InterQual® criteria states that only day one clinical can be used to meet Episode Day One criteria in Adult Acute Subsets. Due to receiving additional days in the initial documentation for clinical review, the primary reviewer may use all clinical received from that hospital stay for the Episode Day One review.
Episode Day One
Residential Treatment Center (RTC), Long Term Acute Center (LTAC), Subacute/Skilled Nursing Facility (SNF), Acute Rehab admission.
Exception: In addition to clinical received on date of admission, we will accept clinical obtained up to three days prior to admission date. Clinical information obtained greater than three days prior to admission will not be utilized by BCBSND primary nurse reviewer for initial determination.
Applied Behavior Analysis (ABA) supervision
Exception: Due to access and geographic barriers, some ABA facilities may only employ Board Certified Behavior Analyst (BCBA) and do not have behavior specialists providing care. If a BCBA provides all direct treatment for the case and does not have a direct services professional to supervise, the supervision requirement will be waived. Documentation will be needed that the BCBA provides all care.
Urgent Home Health-Initial Evaluation
Exception: Discharges from inpatient hospital or Long-Term Acute Care (LTAC) facilities with an urgent request to complete a home health evaluation within 24-48 hours of discharge due to the medical complexity of the patient, can be allowed by nursing staff without InterQual® review based on conversation with the receiving facility regarding medical need.
When the primary reviewer determines the medical necessity is not supported by the criteria, the case is sent to secondary review. Secondary review is performed by a physician or like specialty. The physician can utilize the documentation provided as well as scientific evidence, professionally recognized standards of health care and expert opinion to make a determination on the case.