Member identification (ID) cards contain important membership and coverage information to help you correctly verify benefits and route your claims. Be sure to verify eligibility and benefits prior to rendering care.
Member Identification Card Quick Reference Guide
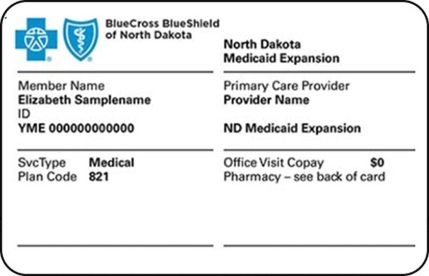
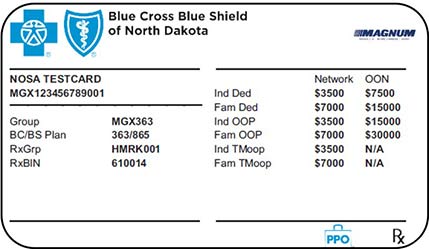
Front of card
Information displayed on cards may vary by plan type, but they all have similar information. Below is a quick reference guide on where to find pertinent details for a member.
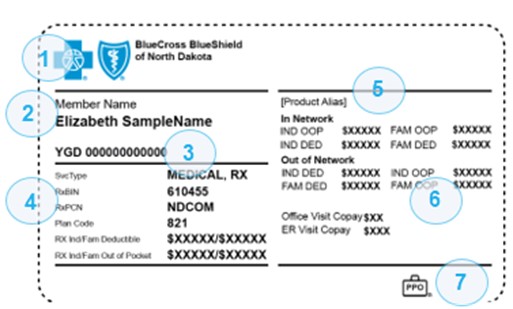
1
Plan logo
2
Subscriber's name
- Plastic ID cards will only display subscriber name. They will not show specific names of covered spouses and/or other dependents unless that member has a digital card from the BCBSND member portal.
3
Unique Member Identification (UMI) ID number. The 3 letter alpha Prefix will vary by plan type.
4
Depending upon plan type, this section may include:
- Svc Type—types of services associated with this card, medical or prescription.
- If a member has dental and/or vision coverage, they will have a separate ID card.
- RxBin, RxPCN, RX cost share—for pharmacy related services
- Plan Code—where to bill the services.
- Office Visit Copay and ER Visit Copay
- Note, this may display in other areas, such as placement #6 depending on plan type.
- Plan network name and information
- Note, this information may appear in placement #5 depending on plan type.
5
Plan network name and PCP, if applicable, e.g., Medicaid Expansion
6
Cost Share information
- Cost share information may include, deductible (DED), out of pocket (OOP), and copay information, when applicable.
- Copay – Amount a member pays up front prior to receiving services.
- DED – Amount owed by member for health care services before insurance begins to pay.
- OOP – Maximum amount member pays out of pocket in a calendar year before health insurance begins to pay 100% of the allowed amounts. This may also appear as TMOOP, which is abbreviated for total maximum out of pocket.
- Abbreviations for type of coverage may vary:
- IND - Individual
- ESP - Employee + Spouse
- ECH - Employee + Children
- E1D - Employee + 1 Dependent
- FAM - Family
- You can use Availity Essentials to verify members level of coverage. More information on this process can be found here under the Eligibility and Benefits section.
7
BlueCard program identifier
Logo
An empty suitcase icon:
What it means
Member has out-of-area coverage that is not a PPO product. Because there are different benefit plans represented by the empty suitcase logo, always verify eligibility and benefits.
A suitcase icon with PPO inside:
Member has PPO (Preferred Provider Organization), or EPO (Exclusive Provider Organization) benefits available for medical services received in or outside the U.S.
A suitcase icon with BlueHPN inside:
EPO Members with access to the Blue High-Performance Network
A suitcase with PPO B inside:
The member has access to a PPO network, referred to as BlueCard PPO Basic.
No suitcase
Cards for governmental programs such as Medicaid or Medicaid Expansion may not have a suitcase. Government determined reimbursement levels would apply to these types of products.
* The suitcase logo is not required on ID cards for members who do not have benefits outside of their Home Plan’s service area. Always verify the members Eligibility and Benefits prior to rendering services.
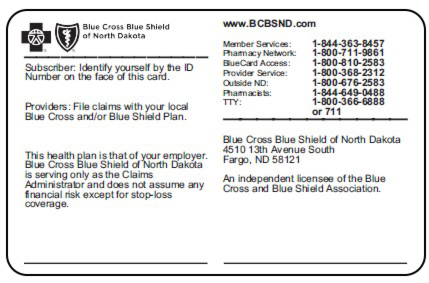
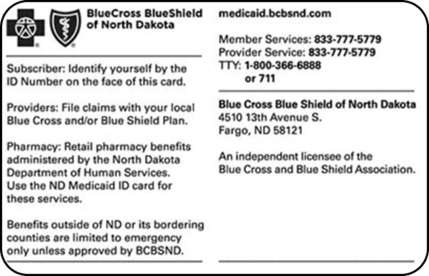
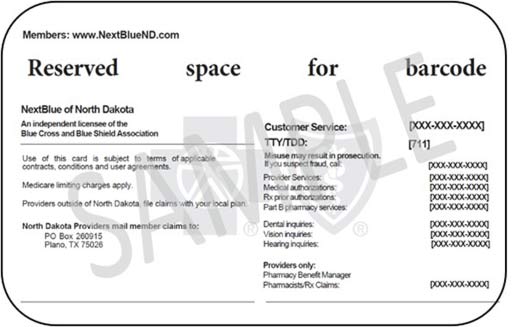
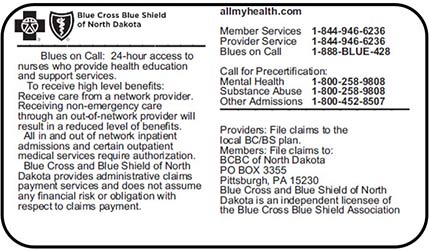
Back of card
The back of the member ID card includes contact information for members, as well as instructions and an address for filing claims and sending correspondence.
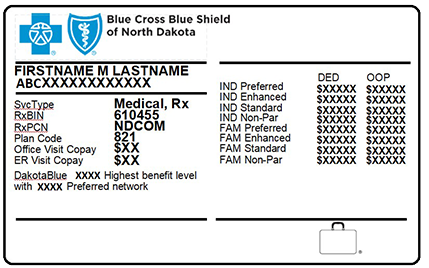
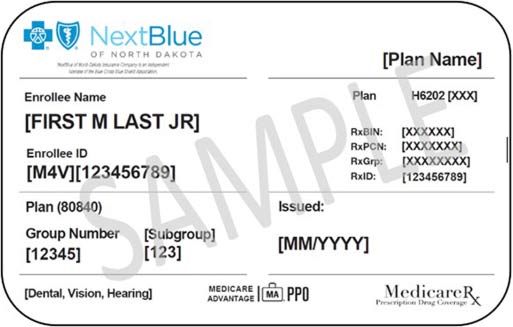
Additional Card Image Examples
As noted above, cards may vary by plan type, here are a few additional examples for reference.
Commercial ID card example
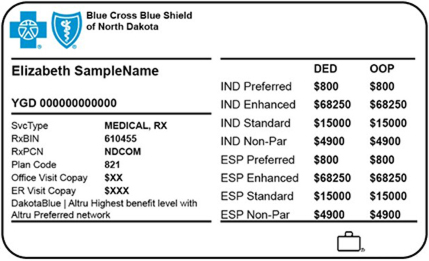
DakotaBlue card example
Medicaid Expansion ID card example
NextBlue of North Dakota ID card example
BCBSND plan(s) administered by Highmark
FEP
Call us with Questions
For questions, call:
BCBSND Provider Service - 800-368-2312
BCBSND Medicaid Expansion Provider Service - 833-777-5779
Federal Employee Program (FEP) - 800-548-4026
NextBlue of North Dakota - 844-753-8039
BlueCard Eligibility line - 800-676-2583