Blue Cross Blue Shield of North Dakota (BCBSND) wants to remind providers to utilize the self-service tools available for precertifications.
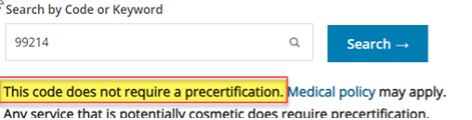
Requests to Utilization Management (UM) or the Customer Contact Center (CCC) for CPT codes that do not require authorization may cause delays in your patient receiving or being scheduled for services. It is important to BCBSND that we continue to meet our timely requirements for precertifications. When reviewing CPT codes that do not require precertification, it becomes harder for the teams at BCBSND to meet those requirements.
On average our UM team receives 1,054 authorization requests a month that do not require authorization. Our Commercial CCC receives on average 60 calls a day, questioning if authorization is required for a specific service.
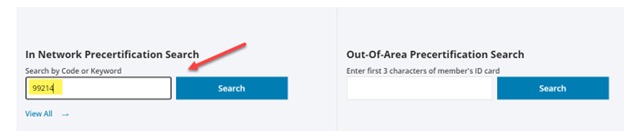
Self-service tools are available to providers to verify if a CPT code has additional steps that need to be taken, i.e., submitting an authorization request or checking medical policy criteria. Steps on how to utilize the Precertification Search tool are below.
Moving forward, we ask providers to ensure precertification(s) is complete prior to claim submission. Providers can utilize the precertification search tool on the BCBSND website to verify which services require precertification. Precertification instructions are listed on this page as well.
Claims submitted without precertification review will be denied, and no additional post-claim review will be completed. This may result in providers being held liable for charges.
How to use the Precertification Search tool:
1. Go to www.bcbsnd.com
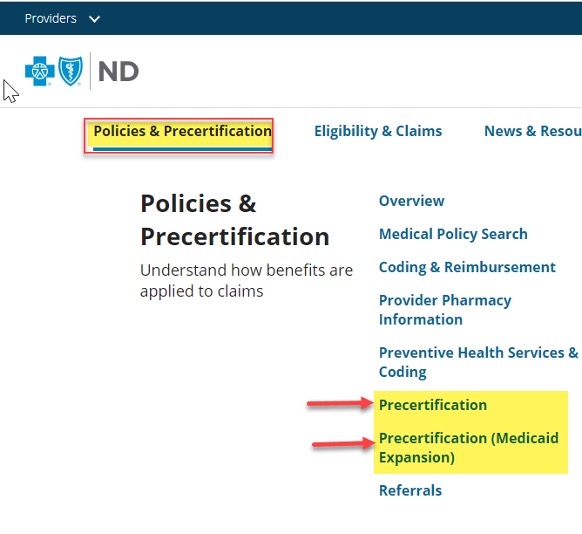
2. Click on Policies & Precertification
3. Then select Precertification for the appropriate line of business. For your convenience they are linked here.