Is a Precertification Required?
On average, our UM team receives more than 1,000 precertification requests per month that do not require authorization. Our Commercial CCC receives on average 60 calls a day, questioning if authorization is required for a specific service.
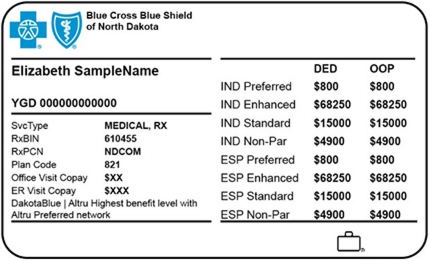
Blue Cross Blue Shield of North Dakota (BCBSND) wants to remind providers to use the self-service tools available for checking if precertification is required for a service. Precertification, authorization, prior authorization, prior approval and/or preauthorization are interchangeable terms meaning a service gets reviewed prior to the service being performed, when required by insurance.
Requests to Utilization Management (UM) or the Customer Contact Center (CCC) for Current Procedural Terminology (CPT) codes that do not require authorization may cause delays in your patient receiving or being scheduled for services. It is important to BCBSND that we continue to meet our timely requirements for precertification, and when reviewing CPT codes that do not require precertification, it becomes harder for our teams to meet those requirements.
Claims submitted without precertification review will be denied, and no additional post-claim review will be completed. This may result in providers being held liable for charges.
In early 2024, we will be moving to a new self-service authorization tool called PA Checkpoint, beginning with updating our precertification webpages on our BCBSND provider website. Following the website updates, we plan to implement this tool within Availity Essentials, which will work with our new Predictal precertification tool that was implemented in November 2023.