How to get started
1. Enroll as a North Dakota Medicaid 1915(i) provider with the State of North Dakota.
a. Make sure to enroll all affiliated clinics and individual providers who may be rendering services.
b. Enrolled 1915(i) providers choose to offer one or more of the following services: Care Coordination, Respite, Training and Support for Unpaid Caregivers, Non-Medical Transportation, Family Peer Support, Peer Support, Supported Education, Benefits Planning, Pre-Vocational Training, Supported Employment, and Housing Support.
2. Provider groups/agencies also need to enroll in our BCBSND Medicaid Expansion network by contacting our Provider Contracting department at providercontracting@bcbsnd.com.
a. Confirmation from Provider Contracting before proceeding with reviewing eligibility and/or other tasks, is also necessary for this step. See the Contracting and Credentialing section below for more information.
3. Get registered for your portal accounts:
a. Therap if you don’t already have an account.
- Medicaid Expansion requires electronic claim submission. Claim submission is done through Therap. It is important to register as soon as possible to avoid delays in submissions and payment(s). See Section Requirements to submit claims section below for more information.
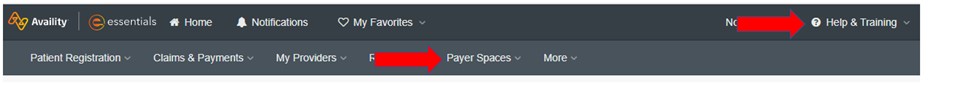
b. Availity if you don't already have an account.
*see section Registering for your portal accounts for more information.
4. Understand the Medicaid Expansion Member ID Card.
a. BCBSND Medicaid Expansion member IDs begin with a YME prefix.
b. Member Identification Card Quick Reference Guide
5. Sign up for HealthCare News (HCN).
a. To subscribe, visit our provider webpage at https://www.bcbsnd.com/providers/news-resources/healthcare-news and click on the Sign up for HealthCare News link. Then enter your email address to start receiving HCN.
b. This allows providers to receive timely information and updates on policies, benefits coding or billing updates, education and more which are delivered directly to your email. We understand not all HCN will apply to 1915(i), so we will put 1915(i) in the article subject or Medicaid Expansion if it reaches beyond 1915(i).
6. Once enrolled with both DHHS and BCBSND, verify the member’s benefit requirements for eligibility to receive 1915(i) services by calling BCBSND at 701-282-1003 during normal business hours.
a. It is the provider’s responsibility to verify a member’s 1915(i) eligibility. Reasons for this include, but are not limited to, a member being eligible for Medicaid Expansion but not eligible for 1915(i) services. A member may lose eligibility for 1915(i) services during their treatment. It is the provider’s responsibility to verify a member’s 1915(i) eligibility.
7. Before working with a member a Care Coordination request must be submitted for a member to be connected with your agency.
a. Use the New Member Care Coordination notification found at https://www.hhs.nd.gov/1915i/providers.
8. Enter the member's plan of care into Therap. See Requirements to provide 1915(i) services below for more details on Therap.
9. Begin submitting claims.
Please note, it is important to understand the documentation requirements prior to rendering services. Information can be found within policies such as, but not limited to 1915i-Provider-Requirements.pdf as noted in the Applicable Guidelines section below, as well as the “Documentation Requirements” section of the Medicaid Expansion provider manual.