Why do some claims require intervention?
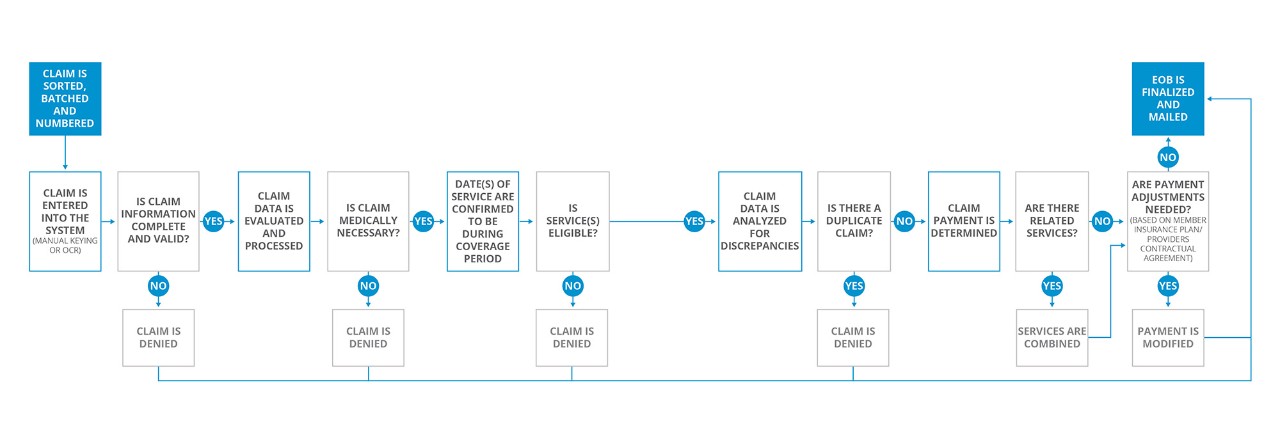
BCBSND maintains 100% claims accuracy. This is because our claims process identifies claims that require intervention. 93% of all claims go through our claims system without any intervention. But what happens to the other 7% of claims? For claims that are held by the system, claims representatives process the claims manually to ensure correct payment. These representatives help make the experience more efficient for you.
How does BCBSND ensure claims processing accuracy?
BCBSND has quality programs that measure timeliness and accuracy to ensure claims are processed correctly. A weekly audit reviews a representative sample of claim submissions, benefit contracts and provider contracts to verify:
- Patient eligibility
- Service eligibility
- Data entry and electronic data integrity
- Claims payment
Exceeding performance standards
As a member of a national association of independently owned Blue Cross plans, BCBSND submits performance metrics to the Blue Cross Blue Shield Association (BCBSA).
BCBSA monitors BCBSND claims performance, ensuring claims processing accuracy meets or exceeds BCBSA performance standards. BCBSND routinely meets or exceeds national averages.